Understanding the Difference Between Bladder Infections and UTIs
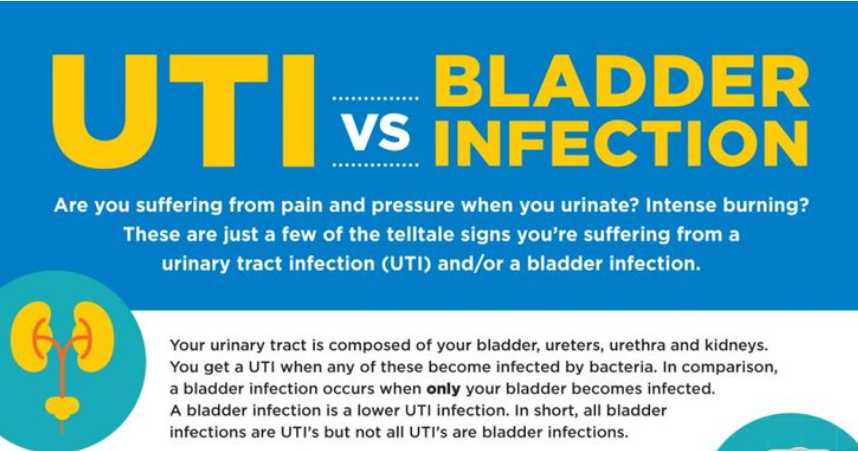
Bladder infections and urinary tract infections (UTIs) are two major forms of infections that affect the urinary system. Although both affect the urinary system, significant distinctions exist between them.
What Defines UTIs and Bladder Infections?
A urinary tract infection, or UTI, refers to any illness affecting the bladder, urethra, ureters, or kidneys. Conversely, a bladder infection specifically refers to an illness confined to the bladder. This means that although all UTIs are bladder infections, not all bladder infections are UTIs.
Recognising Symptoms
The symptoms of UTIs and bladder infections differ. UTIs can cause a range of symptoms, including frequent urination, a strong urge to urinate, discomfort or a burning sensation while urinating, cloudy or bloody urine, and lower abdominal pain. In severe cases, UTIs may also cause chills, fever, and back pain.
Bladder infections typically cause cloudy or bloody urine, a strong need to urinate, and frequent bathroom visits. Although bladder infections and UTIs can share similar symptoms, the severity and extent of symptoms depend on the infection’s location and intensity.
Causes of Bladder Infections and UTIs
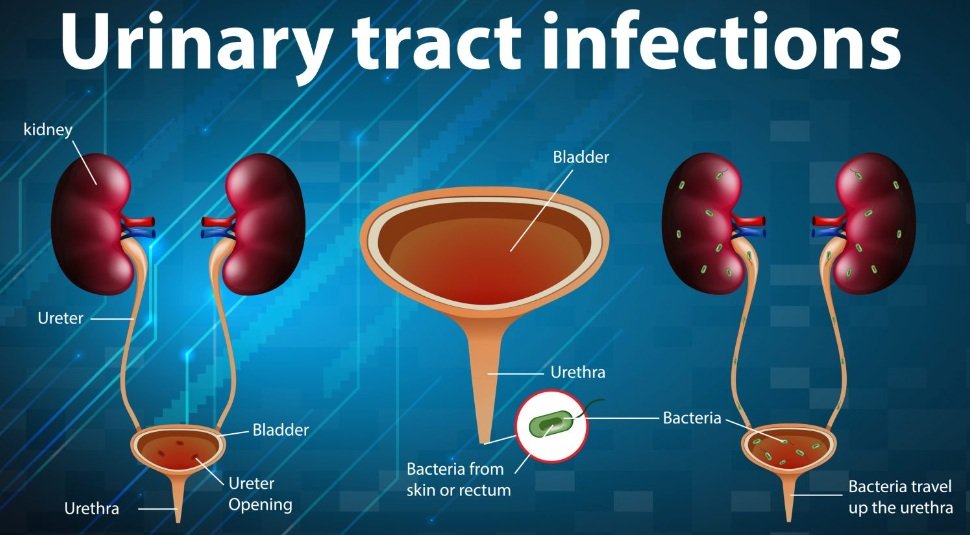
Bladder infections and UTIs have various causes. Bacteria often enter the urinary system via the urethra, causing UTIs. Contributing factors include sexual activity, poor hygiene, and the use of specific birth control methods. In contrast, bladder infections are typically caused by germs that enter the bladder through the urethra. Urinary catheterisation, incomplete bladder emptying, and bladder anomalies can also contribute to bladder infections.
Understanding Urinary Tract Infections (UTIs)
Urinary tract infections (UTIs) are common medical conditions that affect the kidneys, ureters, bladder, and urethra, among other parts of the urinary system. The urinary tract plays a vital role in the body’s waste management system. The kidneys filter blood to produce urine, which passes through the ureters to the bladder. From the bladder, it exits through the urethra. Germ entry, especially Escherichia coli, can result in UTIs.
Types and Symptoms of UTIs
While UTIs can affect any part of the urinary system, the most common types are urethral (urethritis) and bladder (cystitis) infections. Symptoms of a UTI include frequent and urgent urination, a burning sensation while urinating, cloudy or foul-smelling urine, and pelvic pain, particularly in women. In severe cases, UTIs can cause pyelonephritis, or kidney infections, which may result in fever, chills, and back pain.
Women are more likely to experience UTIs due to their shorter urethras, which allow germs to enter the bladder more easily. Other factors that increase the risk of UTIs include menopause, certain birth control methods, sexual activity, and urinary system anatomical anomalies. UTIs are also more common in people with diabetes, weakened immune systems, and urinary catheters.
Diagnosis and Treatment Options
To ensure accurate diagnosis and effective treatment, healthcare professionals typically take several steps when diagnosing bladder infections and UTIs. A thorough medical history and physical examination are usually the first steps in the diagnosis process. Urine sample analysis is crucial in diagnosing these conditions. A urinalysis detects bacteria, red blood cells, and white blood cells, which may indicate an infection. In some cases, a urine culture may be performed to identify the specific bacteria causing the infection and guide antibiotic treatment.
Both bladder infections and UTIs typically require antibiotics as the first line of treatment after diagnosis. The type and duration of antibiotic therapy depend on factors such as the bacteria identified, the patient’s medical history, and the infection’s severity. It is essential to complete the full course of antibiotics, even if symptoms subside before treatment ends, to ensure the infection is entirely eradicated and to avoid antibiotic resistance.
Over-the-counter medications may also be prescribed alongside antibiotics to relieve symptoms such as burning and discomfort during urination. Phenazopyridine is often used to ease pain. Patients are encouraged to drink plenty of fluids, particularly water, to help flush bacteria from the urinary system. Other home management tips include using a heating pad to relieve lower abdominal pain and avoiding irritants like alcohol and coffee.
Prevention Strategies and Lifestyle Changes
Adopting dietary and lifestyle changes to promote urinary tract health is crucial for preventing bladder infections and UTIs. One of the simplest strategies is drinking enough water. Water promotes frequent urination, which helps flush away harmful pathogens from the urinary system and dilutes urine, making it more difficult for bacteria to thrive.
Another important preventive measure is avoiding holding urine for prolonged periods. Holding urine can promote bacterial growth and increase the risk of infection. Always wipe from front to back after urination to prevent urethral contamination from bacteria in the anal region.
Prevention Techniques and Lifestyle Advice
Choosing the right feminine products can significantly affect urinary tract health. Avoid using irritating products such as scented sprays, douches, or powders in the vaginal area, as these can disrupt the natural bacterial balance and lead to infections. Opt for gentle, fragrance-free hygiene products instead.
Diet plays a vital role in urinary tract health. Cranberry juice or supplements can help prevent UTIs by preventing bacteria from adhering to the walls of the urinary tract. Probiotics may help maintain a healthy balance of beneficial bacteria in the body, boosting the immune system’s defence against infections. Foods rich in vitamin C, such as oranges, strawberries, and bell peppers, may help strengthen the immune system and acidify urine, making it less conducive to bacterial growth.
Garment Selection May Impact the Urinary System’s Health
Choosing cotton underwear over synthetic fabrics promotes better air circulation and reduces moisture, which can inhibit bacterial growth. Avoid wearing tight clothing, such as leggings or skinny jeans, as they can trap moisture and create an ideal environment for bacteria.
By incorporating these lifestyle changes and preventive strategies into your daily routine, you can significantly lower the risk of UTIs and bladder infections. This will also enhance the overall health of your urinary tract.