Understanding Pancreatic Disorders
Two different medical disorders that affect the pancreas, an essential organ beneath the stomach, are pancreatic cancer and pancreatitis. Despite the inflammation of the pancreas in both illnesses, the aetiology, symptoms, and available treatments differ.
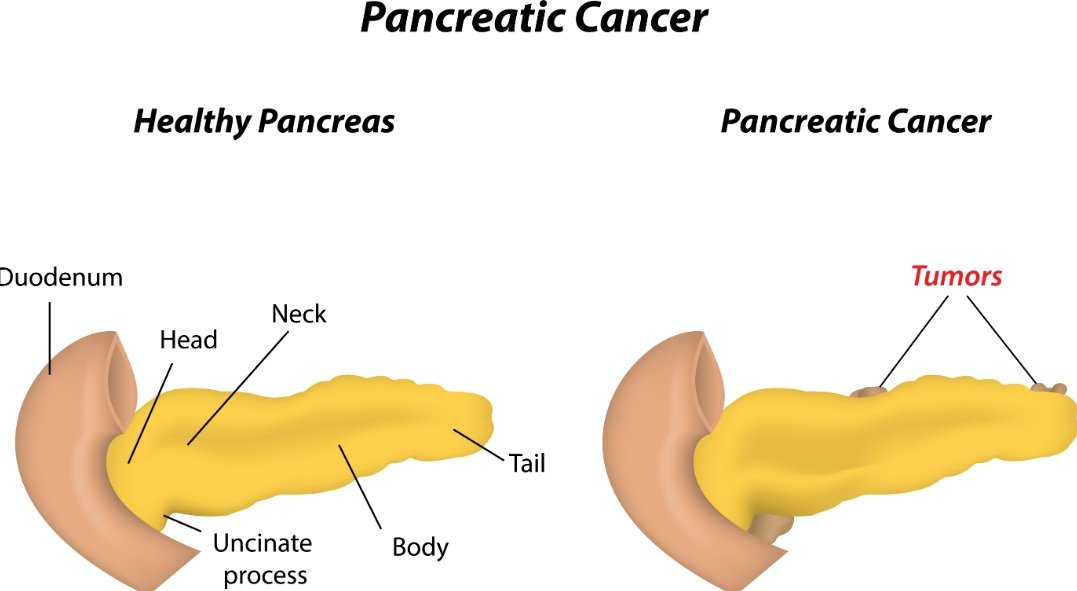
Pancreatic Cancer: A Malignant Condition
The unchecked proliferation of aberrant cells in the pancreas is the hallmark of pancreatic cancer, a malignant condition. It is frequently caused by environmental factors such as obesity, smoking, or a family history of the illness, as well as genetic mutations. Abdominal discomfort, jaundice (yellowing of the skin and eyes), unexplained weight loss, and digestive problems are all possible symptoms of pancreatic cancer. Depending on the stage of the illness, patients with pancreatic cancer may get chemotherapy, radiation treatment, surgery, or a combination of these therapies.
Understanding Pancreatitis: Acute and Chronic
Conversely, pancreatitis, which may be acute or chronic, is the inflammation of the pancreas. Gallstones or binge drinking are the typical causes of acute pancreatitis; however, long-term alcohol misuse or certain genetic disorders are often the causes of chronic pancreatitis. Severe stomach discomfort, nausea, vomiting, fever, and a fast heartbeat are some signs of pancreatitis. In addition to treating the underlying cause of pancreatitis, treatment for the condition includes changing one’s lifestyle to include less fat and alcohol consumption. Hospitalisation and intravenous hydration may be required in extreme situations.
Distinguishing Between Pancreatitis and Pancreatic Cancer
Although pancreatitis and pancreatic cancer both cause inflammation of the pancreas, they vary in their aetiology, signs, and modes of therapy. In contrast to pancreatitis, which is a pancreatic inflammation caused by gallstones or alcohol consumption, pancreatic cancer is a malignant disease caused by abnormal cell proliferation. For an accurate diagnosis and suitable treatment, it is essential to comprehend the distinctions between these two illnesses.
The Role of the Pancreas in Health
The pancreas, hidden beneath the stomach, is an essential organ that is vital to life. Its dual role includes both endocrine and exocrine functions, which means that it is essential for both metabolic and digestive processes. The pancreas is primarily responsible for producing digestive enzymes. These digestive enzymes, which include lipase, amylase, and protease, are essential for digesting proteins, lipids, and carbohydrates in the small intestine and ensuring that the body absorbs and uses nutrients effectively.
Apart from its function in digesting, the pancreas plays a crucial role in controlling blood sugar levels. Insulin and glucagon, two vital hormones, are secreted in order to do this. When blood sugar levels are high, the body releases insulin to let the glucose enter cells for cellular energy generation or storage as glycogen. On the other hand, under low blood sugar conditions, the liver releases stored glycogen into glucose by secreting glucagon, which causes glucose to be released back into the circulation. Sustaining energy levels and overall metabolic health depends on the pancreas maintaining this delicate balance.
The Importance of Pancreatic Health
The pancreas plays several different jobs, so its health is very important. A healthy pancreas ensures efficient digestion and stable blood sugar levels, both of which are required for normal body function. Knowing the significance of the pancreas prepares us to investigate the illnesses that may affect it, such as pancreatic cancer and pancreatitis. Better diagnosis, treatment, and management of both disorders will result from an understanding of their distinctions, even if they affect the same organ.
Understanding Pancreatitis: Acute and Chronic
Pancreatitis: What is it? When a patient has pancreatitis, the pancreas, an important gland beneath the stomach that is vital to digestion and blood sugar regulation, becomes inflamed. Acute and chronic pancreatitis are the two main manifestations that might occur. Although there is inflammation of all kinds, there are differences in the ways that it starts, goes on, and could become worse.
Acute Pancreatitis: Sudden Inflammation
Acute pancreatitis is an unexpected inflammation that usually goes away in a few days with the right medical care. Drugs, excessive alcohol consumption, and gallstones that block the pancreatic duct are all possible causes. Severe stomach pain, nausea, vomiting, and fever are some of the signs and symptoms of acute pancreatitis. These symptoms usually need rapid medical treatment, and imaging tests like CT scans or ultrasounds, as well as blood tests that show increased levels of pancreatic enzymes, are used to confirm the diagnosis.
Chronic Pancreatitis: Persistent Inflammation
Conversely, chronic pancreatitis is a persistent inflammation that may cause irreversible harm and scarring to the pancreas. Acute pancreatitis recurring bouts, autoimmune illnesses, and hereditary factors are among the various reasons for it, while persistent alcohol misuse is the common cause. Malnutrition and ongoing stomach discomfort are common symptoms of chronic pancreatitis due to the pancreas’s decreased capacity to generate digesting enzymes. The diagnosis process for acute pancreatitis is comparable, and further testing to evaluate the pancreas’s functional ability is often used.
Treating Pancreatic Disorders
The goals of pancreatitis treatment are to control symptoms and deal with underlying causes. The first course of treatment for acute pancreatitis may include intravenous fluids to stay hydrated, medication-assisted pain relief, and fasting to relax the pancreas. In extreme situations, measures like surgery or endoscopic gallstone removal may be required. Treatment for chronic pancreatitis mostly consists of pain management, enzyme supplements to help with digestion, and dietary and lifestyle changes that include cutting down on alcohol and eating a low-fat diet.
Understanding Pancreatic Cancer
One kind of cancer that starts in the tissues of the pancreas—an organ located behind the bottom portion of the stomach—is called pancreatic cancer. Adenocarcinoma is the most common kind of pancreatic cancer, making up around 95% of cases. This illness is distinguished by the development of malignant tumours. Adenocarcinomas originate from digestion-promoting, enzyme-producing exocrine cells.
Diagnosing Pancreatic Cancer
There are several different ways to diagnose pancreatic cancer, and most of them combine. Imaging tests like CT and MRI scans are often used to see the pancreas and find tumours. To confirm the diagnosis, a biopsy is required, which entails removing a small sample of pancreatic tissue. Additionally, useful information may be obtained from blood testing, notably from assessments of tumour markers such as CA 19–9.
Treating Pancreatic Cancer
The stage, location, and general health of the patient all influence the treatment choices for pancreatic cancer. For individuals with localised tumours, surgical intervention—such as the Whipple procedure—may be an option. To target cancer cells and reduce tumour size, chemotherapy and radiation treatments are often used. Furthermore , targeted medicines are playing a bigger role in the therapy landscape since they concentrate on certain genetic abnormalities seen in cancer cells.
Key Differences Between Pancreatitis and Pancreatic Cancer
It is crucial to recognise that, despite the fact that both pancreatic cancer and pancreatitis affect the pancreas, they differ greatly in terms of their aetiology, symptoms, modes of diagnosis, available treatments, and prognosis. For efficient diagnosis and treatment, it is essential to recognise these variations.
Causes and Symptoms
Pancreatitis and pancreatic cancer have very different causes. The main causes of pancreatic cancer include exposure to specific chemicals, smoking, genetic alterations, and chronic inflammation. Conversely, gallstones, excessive alcohol use, certain drugs, and metabolic abnormalities are often associated with pancreatitis, which may be acute or chronic. Targeted preventive and treatment initiatives depend on an understanding of these underlying causes.
Pancreatic cancer and pancreatitis can present with different symptoms. Jaundice, unexplained weight loss, and back-radiating abdominal discomfort are common, ambiguous signs of pancreatic cancer. On the other hand, fever, nausea, vomiting, and abrupt, intense stomach pain are usually the first signs of pancreatitis. These symptomatic differences may serve as a guide for healthcare practitioners conducting their first clinical exams.
Diagnostic Techniques and Treatment Modalities
The diagnostic techniques used for these illnesses are specific to their characteristics. In addition to biopsy methods to confirm malignancy, imaging modalities, including CT, MRI, and endoscopic ultrasonography, are often used to diagnose pancreatic cancer. Imaging investigations are used in conjunction with blood tests to detect high levels of pancreatic enzymes and structural abnormalities or inflammation in the pancreas, both of which are critical components in the diagnosis of pancreatitis.
Pancreatic cancer and pancreatitis have quite different treatment modalities. Targeted medication therapies, radiation therapy, chemotherapy, and surgery are some of the treatments for pancreatic cancer that try to eradicate or stop the spread of malignant cells. On the other hand, the therapy for pancreatitis focuses on controlling the condition’s symptoms and resolving its underlying cause. This may include intravenous fluids, pain relief, fasting, and, in some situations, surgical treatments to remove blockages.
Prognosis
Additionally, each illness has a different prognosis. Because pancreatic cancer usually manifests late and is aggressive in character, the prognosis is frequently dismal. Though early discovery may help, this is still one of the most difficult tumours to cure. When treated appropriately, pancreatitis, especially the acute kind, usually has a better prognosis, but chronic pancreatitis needs continuous care and may result in long-term consequences.
For both illnesses, it is critical to identify symptoms early and get medical attention quickly. It is possible to improve patient outcomes by facilitating timely diagnosis and proper treatment by being aware of the differences between pancreatic cancer and pancreatitis.
Table of Differences between Pancreatic Cancer and Pancreatitis
| Characteristic | Pancreatic Cancer | Pancreatitis |
|---|---|---|
| Definition | A malignant tumour in the pancreas | Inflammation of the pancreas |
| Cause | Genetic mutations, smoking, obesity, age, and family history | Alcohol consumption, gallstones, certain medications, trauma, and infections |
| Symptoms | Abdominal pain, weight loss, jaundice, and digestive issues | Severe abdominal pain, nausea, vomiting, fever, and rapid pulse |
| Diagnosis | Imaging tests (CT scan, MRI, ultrasound), biopsy | Blood tests, imaging tests, and pancreatic function tests |
| Treatment | Surgery, chemotherapy, radiation therapy, and targeted therapy | Fasting, pain management, IV fluids, dietary changes, medication |
| Prognosis | Poor; often diagnosed at advanced stages with low survival rates | Generally good with treatment, but may lead to complications |
| Risk Factors | Smoking, obesity, age, family history, and certain genetic syndromes | Alcohol abuse, gallstones, certain medications, and infections |
| Prevalence | One of the most lethal cancers is relatively rare but deadly | Common, affecting millions of people worldwide |
| Progression | Can spread to other organs and tissues (metastasis) | May lead to chronic pancreatitis or complications like pancreatic pseudocysts |
| Screening | No routine screening; diagnosed based on symptoms and tests | No routine screening; diagnosed based on symptoms and tests |