Understanding Endometriosis and Uterine Fibroids
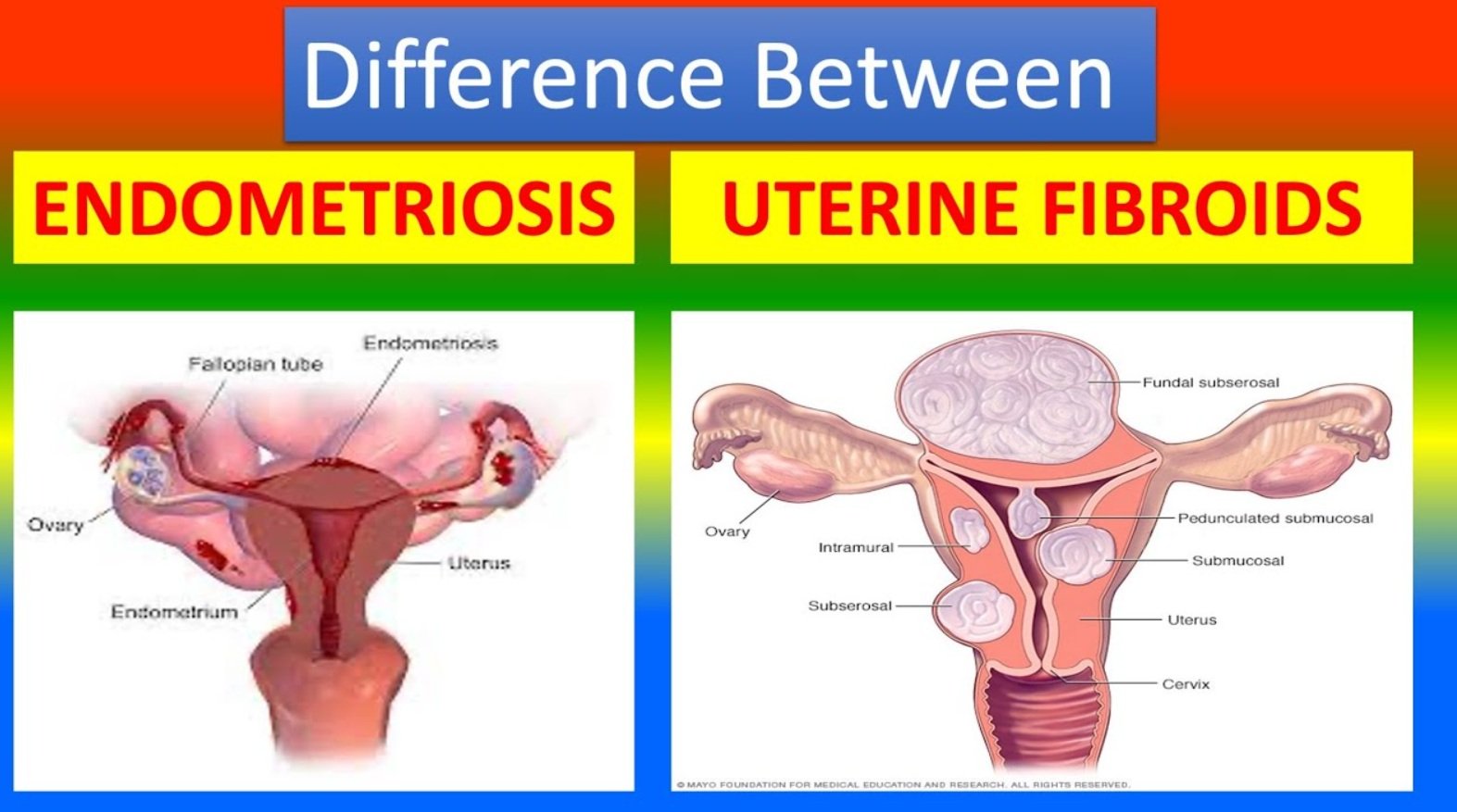
There are two different medical disorders that impact the female reproductive system: endometriosis and uterine fibroids. Endometriosis is a syndrome in which tissue resembling the lining of the uterus develops outside of the uterus, while uterine fibroids are non-cancerous growths that form within the uterus.
Symptoms and Effects
Uterine fibroids, which may vary in size and quantity and cause symptoms including heavy monthly flow, pelvic discomfort, and frequent urination, are generally benign tumours. However, endometriosis may result in infertility, painful periods, and severe pelvic discomfort. Both disorders may have an adverse effect on a woman’s quality of life and may need to be managed with medical assistance.
Diagnosing and Differentiating
Although endometriosis and uterine fibroids might have certain symptoms in common, such as pelvic discomfort and excessive monthly flow, they are two separate diseases with different origins and approaches to therapy. It is crucial that women who exhibit symptoms of either illness see a doctor in order to get a proper diagnosis and treatment plan. Getting advice from a healthcare professional may help you decide what steps to take to manage your symptoms and enhance your general health and wellbeing.
Characteristics and Impact
Endometriosis and uterine fibroids are two common but different gynaecological disorders that impact a large number of people globally. For an accurate diagnosis and successful treatment, it is essential to recognise the distinctions between these two illnesses. Known by other names, such as leiomyomas or myomas, uterine fibroids are non-cancerous growths that originate within the uterus’s muscular wall.
These growths may appear as a single fibroid or in clusters, and their diameters can range from microscopic to several inches. Fibroids may produce a variety of symptoms, such as heavy menstrual flow, pelvic discomfort, and pressure on the bladder or intestines, even though they are usually benign.
Complexities and Challenges
Endometriosis is a disorder in which tissue outside the uterine cavity resembles the endometrium, the uterine lining. Other pelvic organs, such as the ovaries, fallopian tubes, and the outside of the uterus, may become attached to the ectopic tissue. In contrast to fibroids, endometriosis may cause problems, including infertility, and is often linked to persistent pain, especially throughout the menstrual cycle. Endometriosis symptoms may range greatly in intensity, with some women just slightly uncomfortable and others in excruciating agony.
 Prevalence and Misunderstandings
Prevalence and Misunderstandings
Endometriosis and uterine fibroids are both common disorders; research indicates that 10% of women of reproductive age have endometriosis and that up to 70% of women may acquire fibroids by the time they are 50. These illnesses are common, but they are often misdiagnosed or misunderstood, which emphasizes the need for education and awareness campaigns. Women who are able to differentiate between endometriosis and uterine fibroids are more equipped to make health-related choices and seek the right medical guidance and care.
Identification and Diagnosis
Numerous women suffer from uterine fibroids and endometriosis, which can cause severe pain and health issues. Effective management and treatment of these illnesses depend on the ability to identify the symptoms and comprehend the diagnostic processes.
Risk Factors and Causes
Leiomyomas, another name for uterine fibroids, are benign growths in the uterus. Frequent signs and symptoms include pelvic pressure or discomfort, as well as excessive monthly flow, which may cause anaemia. Additionally, some women may feel constipation if the fibroids are pushing on the intestine or frequent urination if the fibroids are pressing on the bladder. Fibroids can also sometimes result in painful sex and protracted menstrual cycles.
Understanding Causes and Risk Factors
In contrast, endometriosis is a disorder in which tissue that resembles the lining of the uterus develops outside of it. This can cause chronic pelvic discomfort, which is often worse during menstruation. Infertility, painful periods (dysmenorrhea), and discomfort during or after sexual activity are among the other symptoms that women with endometriosis may have. Furthermore, endometriosis can cause heavy bleeding, known as menorrhagia, during or between periods, as well as discomfort during bowel movements or urine, particularly during menstrual cycles (menometrorrhagia).
Diagnosis and Evaluation
A mix of physical exams, imaging studies, and medical histories are used to diagnose these diseases. Because an ultrasound can quickly identify the presence and size of uterine fibroids, it is usually the first imaging test done for this type of condition. To offer a more in-depth picture, an MRI scan may be necessary in some circumstances. In order to rule out other illnesses and check for anaemia from significant bleeding, blood tests may also be performed.
Complex Diagnosis and Treatment
Endometriosis diagnosis is more complicated and often begins with a pelvic exam to look for anomalies. Although it may be used, an ultrasound is not usually a reliable tool to find endometriosis. Finding the location and degree of endometriosis may be aided by an MRI. Nonetheless, a laparoscopy—a surgical technique in which a camera is introduced into the pelvic cavity to directly see and sample the endometrial tissue—is often required to get a conclusive diagnosis.
Understanding Reasons and Risks
For an early diagnosis and successful treatment of endometriosis and uterine fibroids, it is essential to comprehend their underlying causes and risk factors. Endometriosis and uterine fibroids are two distinct disorders, but they share a complex aetiology influenced by numerous variables.
Genetic and Hormonal Influences
Hormonal and genetic variables are important in the development of uterine fibroids, which are non-cancerous growths in the uterus. Research points to a genetic connection between fibroids and an increased risk of getting the illness in families with a history of the disorder. Hormonal imbalances, including high levels of progesterone and oestrogen, are also intimately linked to the development of fibroids.
These hormones promote uterine lining growth, which may aid in the development of fibroid tumours. Environmental variables, such as nutrition and lifestyle, may also increase the risk, though this is less well understood.
Underlying Factors and Associations
Endometriosis, on the other hand, causes discomfort and may interfere with conception because it is defined by the formation of endometrial-like tissue outside the uterus. Retrograde menstruation, in which menstrual blood travels backward via the fallopian tubes and into the pelvic cavity, is one well-known explanation of its aetiology. After that, the dislodged tissue develops and implants outside the uterus.
Furthermore, immune system abnormalities may prevent the displaced endometrial cells from being identified and eliminated, enabling them to multiply. Another reason is genetic susceptibility; studies show that those with a family history of endometriosis have a greater prevalence of the disorder.
Impact of Age and Ethnicity
Age is a common risk factor for endometriosis and uterine fibroids, with women of reproductive age often being diagnosed with the condition. Other common risk factors include ethnicity, obesity, and the early start of menstruation, as these disorders are more common in certain racial groups. Notably, endometriosis is often found in women with a history of pelvic infections or other uterine abnormalities, while uterine fibroids are more prevalent in African American women.
Customized Approaches to Treatment
Treatment options for endometriosis and uterine fibroids differ greatly depending on the patient’s symptoms, level of severity, and reproductive objectives. First-line therapy is often medical, with the goal of reducing endometriosis lesions, fibroid size, and symptoms. Hormone treatment, such as gonadotropin-releasing hormone (GnRH) agonists and antagonists, works by reducing oestrogen levels to successfully decrease the size of fibroid tumors and control pain associated with endometriosis. Painkillers and nonsteroidal anti-inflammatory medicines (NSAIDs) are often administered to treat both disorders’ accompanying pain.
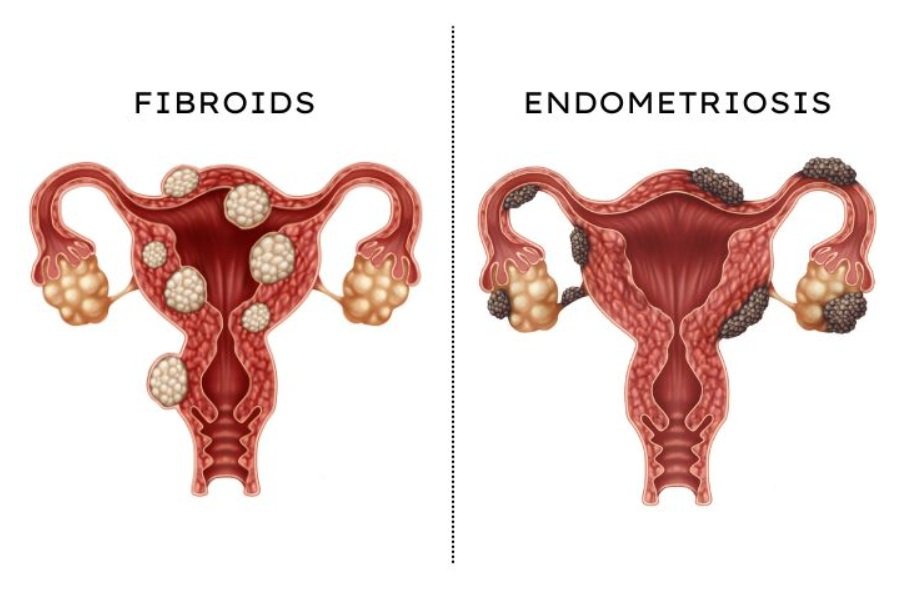 Table of Differences between Uterine Fibroids and Endometriosis
Table of Differences between Uterine Fibroids and Endometriosis
| Characteristic | Uterine Fibroids | Endometriosis |
|---|---|---|
| Location | Grow inside or on the uterus | Grow outside the uterus, affecting nearby organs |
| Cause | Exact cause unknown; hormonal and genetic factors may play a role | Endometrial tissue grows outside the uterus, possibly due to retrograde menstruation or immune system dysfunction |
| Symptoms | Heavy menstrual bleeding, pelvic pressure, frequent urination | Pelvic pain, painful periods, infertility, painful intercourse |
| Diagnosis | Ultrasound, MRI, pelvic exam, hysteroscopy | Laparoscopy, pelvic exam, ultrasound, MRI |
| Treatment | Medications, surgery (myomectomy, hysterectomy) | Medications (pain relievers, hormonal therapy), surgery (laparoscopy, hysterectomy) |
| Complications | Infertility, anemia, urinary tract infections | Infertility, ovarian cysts, bowel obstruction |
| Prevalence | Common, affecting many women during their reproductive years | Common, affecting about 10% of women of reproductive age |
| Growth | Slow-growing benign tumors | Endometrial tissue grows and sheds outside the uterus with each menstrual cycle |
| Associated Conditions | Anemia, urinary problems | Chronic pelvic pain, ovarian cysts |
| Management | Often managed with watchful waiting or symptom management | May require long-term management and monitoring, including pain management and fertility treatments |



